A team of Johns Hopkins materials science and engineering undergraduates has designed a new artificial heart valve—specifically for the mitral valve in the heart’s left side—that doesn’t require stitches. Their innovative design uses a flexible nickel-titanium alloy mesh that expands to push against the surrounding tissue, potentially making heart surgeries simpler and safer for patients.
The students will present their concept on April 29 at the Whiting School of Engineering’s Design Day—an annual event showcasing students’ solutions to real-world problems.
“A mitral valve replacement is rather typical in heart surgeries but very time-consuming because placing sutures to secure the prosthesis can take up to an hour,” says team leader Vara Gunananthan. “During this time, the heart is on bypass, and the longer this process takes, the more risks there are with the surgery. Making an effective sutureless mitral valve replacement would solve these issues.”
During their research, the students found that their artificial valve would need to be versatile enough to fit a range of irregular valve shapes caused by calcification—a common condition where calcium builds up on heart valves, stiffening them and making them less effective.
“Calcification causes the valve and surrounding tissue to harden. It affects the valve and the area of the heart around it and is a regular problem surgeons find with the mitral valve,” says Gunananthan. “Our prosthesis must conform to the shape of calcified valves and push against them with enough force to secure itself against the pressure of the heart pumping.”
Because the causes of calcification are not well understood, the team developed its own methods to simulate the condition to test how their prosthesis would perform in calcified tissue.
“We made calcification models by placing a combination of Borax crystals and gravel in silicone, mimicking the tissue calcification we see on a CT scan, so we could test our prosthesis model,” says Gunananthan.
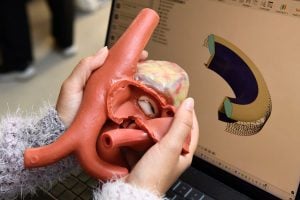
The team then created a model of a prosthesis that uses a bumper to conform to the heart’s varied internal shapes and a sleeve to house a mesh support ring. For the mesh, they used an alloy called nitinol—a nickel-titanium material known for its superelasticity, which is the ability to return to its original shape. In their computer-assisted design (CAD) model, the nitinol mesh surrounds the prosthesis and is designed to expand inside the body, pressing against the tissue to hold it in place. The team then built a physical prototype of the prosthesis based on this digital model.
“The difference between our models and what is currently on the market is how the prosthesis deploys and presses against the tissue surrounding the valve,” says Gunananthan. “The interior of our prosthesis will be the same as others, but the structure around it will set it apart and allow for a swift replacement surgery without the need for sutures.”

The students plan to test their CAD model using COMSOL Multiphysics simulation software to ascertain how well nitinol would work in a calcified mitral valve.
“We have a good idea about how this would work based on our computer designs and simulations, but our physical design uses copper wire instead of nitinol because the alloy continues to expand with heat and is difficult to work with,” says Gunananthan. “Moving forward, we want to find a manufacturer to produce the nitinol mesh with the prosthesis so we can test our simulations in real life.”
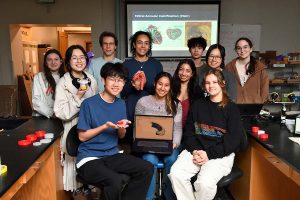
Team members include materials science and engineering students Tyler Lee, Veronica Ivanovskaya, Andrea Wat, Andrew Kim, Admy Palacios-Gonzalez, Sophia Cheng, Alex Yau, and Karina George. The work was done under the mentorship of assistant research professor Thomas Garrison and Michael Robich, Regional Medical Director of Cardiovascular Services in the Western Division for Banner Health and fellow-in-courtesy of the Department of Materials Science and Engineering at Johns Hopkins University