A biomedical start-up across the street from the Homewood campus —IBT—is creating lifesaving products that draw upon faculty and alumni expertise.

Like a good novel, the story behind Infinite Biomedical Technologies (IBT) begins with an intriguing partnership—between a self-professed “high school drop-out” and a scientist straining to hear the music of the human brain. To date, their collaboration has led to the development of a promis– ing portfolio of biomedical devices—several of which have lifesaving potential. What’s more, in just five years of operation, their Baltimore-based company has raised more than $3.7 million, nearly one-third of which is invested in collaborative investigations with Hopkins researchers, including the Department of Biomedical Engineering. And co-founded by a Whiting School alumnus, IBT has already provided opportunities for other alumni to become involved in creating advanced biomedical products.
But before we reveal the plot, let’s first introduce the principal characters.
The CEO: Ananth Natarajan, MD, ’92 MSE
He was anything but your average teenager. The son of a cardiologist and a nephrologist, Ananth Natarajan decided at the age of 14 to drop out of high school—not to go to work, but to enroll at nearby Duke University. Having attended Duke’s pre-college program, he felt he was ready for college. Duke agreed, and after he double-majored in biomedical and electrical engineering, he graduated with distinction in 1990 at age 18.
That was only the beginning of pursuing his studies—and his vision. “When I was starting my senior year at Duke, having grown up around physicians, I saw there was a pretty big chasm between engineering and medicine,” Natarajan recalls. “Although there were a lot of great technological discoveries being made in the late ’80s, there wasn’t really a good mesh with actual applications in clinical medicine. With that in mind, I decided I wanted to develop a career that bridged the two.”
Natarajan’s advisors recommended the Whiting School to help him merge these two interests. “They told me that Hopkins was the best institution in the world when it came to applying engineering principles to the practice of medicine,” he says. Arriving at Hopkins for a visit in 1989, Natarajan met with Nitish Thakor, professor of Biomedical Engineering and chief investigator at the Biomedical Instrumentation Laboratory. The chemistry between the two was immediate. “I explained to him my vision for applying engineering to real-world clinical problems, and he was very excited by that,” Natarajan recalls. “He suggested that I work with him while getting my graduate degree.”
“There’s a value to being next to a university campus. This could be the beginning of a industrial park or an incubator. Why not here?” NITISH THAKOR

The Scientist: Nitish Thakor
One of the first things you notice about Thakor is his dry, understated sense of humor. However, bring up the topic of his life’s research, and his passion about the subject becomes readily apparent. “There was a time when we didn’t worry about the brain because we had to worry about the heart,” he says. “Now, heart attacks can be handled. So, the brain has become the next frontier, which is why I work on it.”
Thakor’s area of expertise and research is neuroengineering, an emerging field defined by its use of engineering, computational, and mathematical approaches to solving problems in clinical neurosciences (the medical study of the human brain and nervous system). The central focus of Thakor’s lab is on developing a host of solutions—such as new and advanced sensors, instrumentation, micro- and nanotechnologies, and signal processing algorithms— that will lead to technology development and practical clinical applications for neurological use. “We take projects from basic research to commercial applications and research solutions from ‘bench to bedside,’ ” says Thakor. “After 10-15 years of basic research and development, here we are on the threshold of clinical use on patients in lifesaving situations. The university-industry partnership is the one that is making it happen. We couldn’t have done this without the Biomedical Engineering Department and the Whiting School. There’s a value to being next to a university campus. This could be the beginning of a industrial park or an incubator. Why not here?”
Hatching Ideas: The First Stage
Natarajan spent two years at Hopkins, earning his master’s in biomedical engineering in 1992. Although Thakor was away on sabbatical during part of this period, Natarajan remembers it as a very productive time. “Dr. Thakor and I actually raised our first offer for seed capital in 1991, with the help of JHU’s Office of Technology Licensing,” he says. “However, I decided that the project and timing were not quite right. I was not quite finished with my education, so we turned down that offer.”
In 1992, Natarajan entered the University of Chicago’s Pritzker School of Medicine, graduating with an MD in 1996. “Throughout that time, I continued to talk with Nitish on a regular basis,” he recalls. “I even spent my first summer during medical school back at Hopkins, working at his lab. We were hatching several different ideas on how we could create a company.”
By 1996, the timing seemed right. After receiving special permission from the American Board of Obstetricians and Gynecologists to complete a part-time residency track leading to certification as an OB/GYN physician, Natarajan returned to Baltimore—with the goal of starting a new company with his mentor, a company assertively named Infinite Biomedical Technologies.
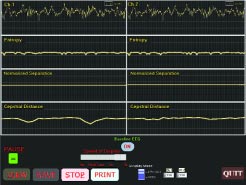
The new company would greatly benefit from Thakor’s expertise. More a decade ago, through his neurological studies, Thakor began to investigate a problem pointed out to him by neurologists and anesthesiologists—that of not being able to understand the rhythms in the brain, especially for the purposes of clinical diagnosis. The human brain, like the heart, is regulated by electrical charges or “signals.” The repeated sequence of these signals forms a recognizable rhythm, which can be monitored and analyzed. Decoding and understanding brain rhythms can be critical in at least two ways, according to Thakor. “One issue is monitoring a patient while under anesthesia, or in an operating room for brain or spine surgery. Another is assessing potential damage when a patient suffers cardiac arrest and blood flow to the brain is interrupted.”
However, identifying brain rhythms (EEGs) is no easy matter. Individual brain signals are minute—one-thousandth the size of a heart signal. “What’s more,” say Thakor, “the heart is one organ generating a single rhythm sequence, while the brain is a hundred billion ‘hearts’ doing different things. There’s also a lot of noise in the brain rhythm, so isolating and interpreting that message is very challenging.”
Thakor uses a shortcut to integrating and reading brain rhythms through a process called evoked response, in which the brain, given an artificial stimulus, responds with a diagnostic set of rhythms. Still, this manual process can consume precious time when a patient’s life is at stake. “If it takes me 10 minutes before I can interpret a certain brain rhythm,” says Thakor, “that can be too late. It’s like “Name That Tune”—I need to figure out the tune from the first few notes of the evoked response to know whether something has happened.”

Thakor’s research into the basic mechanisms of brain injury, which began under a 1986 grant from the National Institutes of Health (NIH), has led from the creation of mathematical models of neurons and neural networks, to the development of signal processing algorithms for analysis of brain rhythms such as EEG and evoked responses. Still, throughout his investigations, Thakor was nagged by a recurring missing link. “Each time we developed methods to determine the brain rhythms and analyze mathematically how the brain rhythms are changing due to surgery or anesthesia or brain injury, the issue that remained was how to take that from bench to bedside—we never actually built the instrument,” he says. “The underlying premise—that we needed to create a clinical instrument to monitor real patients—remained on the back burner.”
Taking that next step—building an actual device (in this case, a diagnostic monitor for brain injury detection in the operating room and neurological intensive care)—can prove daunting to a researcher with no background in commercial development. “To proceed systematically on this path requires a very different form of engineering development and organizational resources,” says Thakor. “Typically, professors do not do product development research.”
However, by 1997, the solution presented itself: his former student. Natarajan felt likewise: “Even before we founded IBT, Nitish had spent 10 years of hard work unlocking several fundamental discoveries about the brain’s response to injury. His neurological projects played a seminal role in our genesis of the company.”
A Successful Launch
IBT was founded on March 17, 1997. “When we decided to start a company,” Natarajan says, “neither Nitish nor I had any business experience. But we decided to go ahead.” Natarajan already had a number of development ideas; what remained to be found was capitalization.
That same year, Natarajan was invited to NIH to sit in one of the study sections for the Small Business Innovation Research Program (SBIR). “In reviewing those applications, I realized that the program had a lot of potential,” he says. For individuals who want a career in developing biomedical devices, such an opportunity provides “the necessary seed funding to see the ideas flourish,” he points out. “This is particularly important in the medical device arena, where venture capital is typically not invested until a much later stage, due to regulatory and other financial hurdles that small companies in the biotech and medical device arena typically face.”
IBT was awarded its first SBIR grant in 1998, and others quickly followed—to date, the company has received 11 NIH grants, totaling $3.7 million. To put this amazing streak into perspective, the average hit rate for receiving SBIR grants is about 33 percent. However, IBT has had an 80 percent success rate between first submission and first resubmission—that is, four of its five proposals have received funding.
Leroy Nyberg, MD, PhD is well-qualified to speak about IBT’s success. He had overseen one of the company’s grants as Urology Program director at the National Institute of Diabetes, Digestive, and Kidney Diseases, part of NIH. “I was so impressed with what they have done, the people they’ve hired, and products in development even at that early stage,” says Nyberg. “What makes IBT unusual is that many times the president of these companies is not a physician, but is either an engineer or a business person. What makes Ananth more successful is that in addition to his bioengineering background, he’s able to take his clinical expertise and really think of innovative clinical ideas in many areas.” Natarajan “has been very effective in getting funding from many different NIH institutes for many projects, using SBIR. That really attests to his ingenuity, expertise, and vision in developing products. He’s an original thinker who can really take ideas and run with them,” Nyberg states.
Natarajan calls his relationship with NIH “a very rewarding partnership. It has made an enormous contribution to the growth of this company.” Now in its fifth year, IBT has a full-time staff of seven, and is rapidly moving to product development in three key areas:
- Cardiac technology: The company is building the Implantable Myocardial Ischemia Detection Indication and Action Technology (IMMeDIATE). Literally a lifesaving “early warning” device for heart patients, it is a sensor to be used with existing pacemakers; its special signal processing software detects reliably impending myocardial infarctions.
- Gynecology: Stress incontinence can become a debilitating problem for older women. IBT is developing a non-surgical therapy in the form of an artificial urethral sphincter. This Intraurethral Continent Prosthesis (INCOPRO) uses advanced materials and microfabrication (MEMS) technology to create a small implantable valve.
- Neurocritical Care: The fruits of Thakor’s research are being applied to the development of several devices. For example, the Cortical Injury Monitor assesses the extent of brain injury following cardiac arrest. And the Intraoperative Neurological Monitor provides real-time feedback on a patient’s neurological status during high-risk situations.
Fast Learning Curve
For IBT and its founders—and for the company’s continuing partnership with Hopkins—the future looks promising. IBT’s Baltimore headquarters, located on Charles Street at 29th Street, is a short walk from the Homewood campus (IBT also has a satellite office in California). To date, IBT has subcontracted more than $900,000 of research work to faculty in Biomedical Engineering and Neurology. “There have been great benefits on both sides,” notes Thakor. “We’ve received significant funding to support our research, while many of my students have leveraged their association with IBT in launching their careers, or are now working for IBT.” Jeffrey Wallace ’02 MSE and Feras Al Hatib, who was a postdoc fellow in Thakor’s lab, are full-time employees of IBT. Rutwik Ghodadra ’99 MSE; Manan Atit ’98, ’02 MSE; Neda Poomipanit ’02 MSE; Ruchika Singhal ’02 MSE; and Anshul Thakral ’99, ’01 MSE all contributed to furthering the unique relationship between Hopkins and IBT.
Natarajan admits that “our evolution is kind of unique. We are going forward step by step, and we would like to go as far as we can.” Thakor agrees: “We found that business development was not as burdensome or mysterious as we thought. Our learning curve has been really good.”
Lani Hummel, director of the Whiting School’s Office of Industrial Initiatives, is more deliberate in her praise. “To hear Ananth and Nitish talk about their efforts makes it sound easy after the fact, but that would really underestimate how much effort was involved here—and how much of the success of this start-up was dependent upon a very solid symbiotic relationship that is still ongoing,” she says. “At the same time, Nitish and Ananth are very open to partnering with other faculty, and sharing their expertise in moving intellectual property from concept to market. I think it’s of tremendous value to the Whiting School to have a company that is ready and well-equipped to be supportive of our faculty and their entrepreneurial efforts.”
Meanwhile, Thakor is setting up an Entrepreneur’s Club through the Whiting School. Its purpose is to facilitate the exchange of information and lessons learned in an effort to encourage faculty to engage in entrepreneurial activities. “We’d be very interested in talking to alumni and friends who’d like to become involved in mentoring faculty and students in entrepreneurship,” says Hummel.
“We’ve really invested in developing a core competency as a university/industry hybrid, and now it is paying off tenfold.” ANANTH NATARAJAN, MD, ’92 MSE
Natarajan observes that “We’ve really invested in developing a core competency as a university/industry hybrid, and now it is paying off tenfold, both for the company and for Hopkins’ Biomedical Engineering Department. It’s an opportunity to win on all fronts. Financially, it supports great research—we can publish more, pursue patents, and get real products to market.”
For further information on IBT, visit www.i-biomed.com . To learn more about the Entrepreneur’s Club or industrial partnerships with the Whiting School, contact Lani Hummel at [email protected] or (410) 516-8941.




