A research discovery leads to a new lifesaving diagnostic tool—and a new company.
Cardiologists have a problem. When they look at conventional images of the heart, they can’t see a true picture of the motion of the heart muscle. As a result, they cannot detect mechanical strain or deformation, one of the early warning signs of cardiovascular disease.
Jerry Prince believes he has a solution. The key to effective cardiac imaging lies in a closer examination of the “donut,” according to Prince. He is the William B. Kouwenhoven Professor in the Whiting School of Engineering’s Department of Electrical and Computer Engineering, a researcher at the Center for Imaging Science, and co-director of the Image Analysis and Communications Lab.
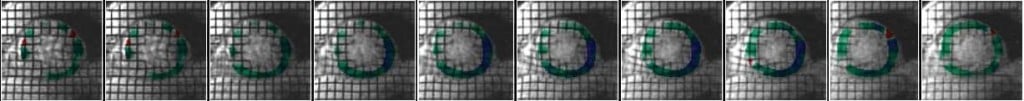
“Imagine a cross-section of the human heart as a donut,” Prince explains. “The thickness of the donut is the muscle, with the hole being where the blood passes. When scanned by most traditional imaging techniques, this area between the two contours on the inside and the outside of the donut is going to be fairly constant in intensity—there’s no resolution to show differentiation of the muscle fibers.”
However, “tagged” magnetic resonance imaging (MRI), developed in the late 1980s, does make possible the capture of such critical detail. Prince says MRI tagging, in which a computer “marks” locations on the heart muscles and then tracks their movements, produces a clearer, more precise picture. “An MRI provides better resolution,” he explains. “You can see details better. With MRI tagging, you can see what’s going on within the walls of a heart muscle. It can image the way the muscle is working. There’s no other technology that can do that now.”
However, this advance in cardiac imaging has had its shortfalls, challenging Prince and his Hopkins colleagues to seek new solutions over the past decade. Simply put, the imaging process in its original configuration was much too slow, and therefore too costly, to be used for regular patient screening tests. “The diagnostic use of tagged MRI is problematic in that you can gather scanned data in a half-hour, but it then takes several hours to process these data,” says Prince. As a result, physicians instead have relied on older imaging techniques like ultrasound for cardiac testing, even though potential problem spots might be missed. To make MRI tagging more useful—and more clinically feasible—a new method of processing the data was necessary. “It was always on my mind that we needed a better way,” Prince recalls.
The Breakthrough Development: HARP MRI

In the late 1990s, Prince and his then-graduate student assistant, Nael F. Osman, found the answer. (Osman, who earned his PhD in 2000 at the Whiting School, is now an assistant professor in the Johns Hopkins School of Medicine’s Radiology Department). The two scientists discovered that the motion of an MRI tagged heart generates an individual signal, which can be captured and decoded through the proprietary software they developed. The result produced high-resolution images like those created by conventional MRI tagging, but at a fraction of the original processing time. Prince and Osman presented a paper in 1999 that announced their new invention: harmonic phase (HARP) MRI. Their new imaging system combined proven MRI tagging technology with rapid processing software.
“HARP MRI is just a very efficient processing method that can take the data you get from a scanner and produce maps of the motion or internal mechanical strain in the heart, which is really the characterization of local muscle deformation,” says Prince. For the first time, there’s now a way to provide the essential missing link to transform MRI tagging into a practical, cost-effective, and potentially lifesaving technology. As a result, notes Prince, “We think it will be a critical component of any cardiac MRI exam.”
While a patient is still inside a magnetic resonance imaging scanner, by using HARP MRI, physicians will have an efficient means of determining whether a heart disorder or damage actually exists. If a problem is found, the immediate availability of images will help doctors decide whether the patient requires surgery or just a change in diet and exercise. In addition, the HARP MRI system can be used to check the effectiveness of new drugs designed to revive stunned heart muscles.
“I think the HARP concept could revolutionize or dramatically change the way we do cardiac stress testing,” says cardiologist Joao Lima, who has used the system. “With it, we can receive quantitative results in a matter of minutes,” adds Lima, who is associate professor of Medicine at the Johns Hopkins School of Medicine. “It allows us to see the degree and extent of the heart problems. There’s nothing else that can do that right now.”
From Inventors to Entrepreneurs
Once word of their new and highly marketable invention spread, Prince and Osman thought commercialization offers would follow in short order. To their surprise, none materialized. “To some extent, we were a bit naïve,” says Prince. “We expected MRI companies to become interested right away. But that wasn’t happening, although there was a growing interest in the research community.”
Faced with the daunting tasks of promoting awareness of their invention, pursuing the next level of research and testing for it, and maintaining the pace of their academic duties, the two inventors hit upon a novel strategy. They would create a company to market HARP MRI while providing licensed beta versions of it to a few select cardiac MRI research groups around the world for evaluation and feedback. To that end, Diagnosoft, Inc. was founded in June 2002.
“We realized that having a company might serve a couple of purposes,” says Prince. “First of all, it would provide a mechanism to get this product out to the research community, and in that way offload some of the burdens from us. Also, it would provide a mechanism for creating a uniform product that we could track and issue revisions for over time. At the same time, we knew that there would be an eventual market out there for HARP MRI if the software were made available. So it seemed the right time to make our software available commercially as well as to qualified researchers.”
New Partners, Next Steps
In less than two years, this initial strategy has paid off. According to Prince, “The top research community is looking at what we’re doing now and wanting to be involved. We have quite a strong following that is working with us to help refine and critique the beta product.” Prince expects his company’s first product, HARP Diagnosoft, to be released in a commercial clinical version sometime over the next year.
In the interim, Diagnosoft itself has grown. Two more partners have joined Prince and Osman, and the company also includes a team of three software developers in Egypt. In addition, Diagnosoft has benefited from the University’s ongoing support through the Whiting School’s Office of Industrial Initiatives. According to Lani Hummel, the office’s director, “ The University is becoming increasingly supportive of faculty who start companies.” Hummel’s office operates as the front line of that support, providing guidance to a range of resources for fledgling companies—from start-up funding from venture capitalists and state organizations to business assistance and marketing development. “These services are valuable for anyone wanting to learn about the process of getting a product out of the University and into the commercial marketplace,” she says.
In the case of Diagnosoft, Hummel notes, “I think that Jerry and Nael have done all the right things to get their company started, and they’ve done everything they need to do to take the company to the next level.” Diagnosoft has an option agreement with the University that allows for start-up time to raise money while testing the prototype technology.
In return, Prince appreciates the University’s role in getting his company off the ground. “I have to give Hopkins a lot of credit for going along with me,” he says. “From the start, they stepped right up and wanted to help and be a partner in this activity. They have supported us throughout the patent process and continue to do their part.”
Looking back at six years of whirlwind change in his professional life, Prince is somewhat amused by the turn of events but decidedly upbeat about his future. “I could have easily come to this point in my career and not have any invention that could be considered marketable,” he admits. “But it was just too compelling not to do it. The entrepreneur thing is new to me, but I find it exciting and rewarding,” he says with a smile. “Ours is a good story—a lot of strong work ethic and at the same time, a bit of luck.”
Snapshot: Diagnosoft’s Two Co-founders

Jerry L. Prince: (left) Chief scientist and chairman of the board for Diagnosoft, Inc. In 1989 Prince joined the Whiting School’s faculty. He is the William B. Kouwenhoven Professor in the Department of Electrical and Computer Engineering and holds joint appointments in the departments of Radiology (School of Medicine), Biomedical Engineering, and Applied Mathematics and Statistics. He also is a researcher at the Whiting School’s Center for Imaging Science and co-director of the Image Analysis and Communications Lab. Prince received a 1993 National Science Foundation Presidential Faculty Fellows Award and was Maryland’s 1997 Outstanding Young Engineer. Together with Nael F. Osman ’00 PhD, he has filed three patents related to MR image analysis.
Nael F. Osman ’00 PhD: (right) Chief technical officer for Diagnosoft. While earning his doctorate at the Whiting School, he co-invented the HARP technique for rapid analysis of tagged MR images with Jerry L. Prince, his research advisor. Osman is now an assistant professor in the Radiology Department of the Johns Hopkins School of Medicine and a talented software systems architect. Prior to studying at Hopkins, Osman helped to develop a voicemail system now being marketed in Egypt.
Visit the Image Analysis and Communications Lab (IACL) at iacl.ece.jhu.edu/ and visit Diagnosoft, Inc. at www.diagnosoft.com
Thanks to Phil Sneiderman for his contributions to this article.
The arrangements discussed in this article have been reviewed in accordance with Johns Hopkins’ conflict of interest policies. Nothing in this article constitutes or implies an endorsement by The Johns Hopkins University of Diagnosoft, Inc., its products, or services.




