Biomedical engineer Jennifer Elisseeff is known for asking bold questions and pursuing seemingly “outlandish” ideas that pay off big. Her latest cross-disciplinary pursuit? Unlocking the mysteries of aging.
Senescent cells are known to accumulate in our bodies as we get older. Though they have stopped multiplying, they remain alive, releasing chemicals that can cause inflammation.
Jennifer Elisseeff believes these cells might hold the key to unlocking a crucial component of the aging process. To find out how, she is looking to an unlikely culprit: fibroids. Largely benign, these muscular tumors grow in the uterus and cause pain and bleeding. Fibroids are packed with senescent cells.
“If you can understand what’s going wrong, you can start blocking it,” says Elisseeff, who is collaborating with researchers in the Department of Gynecology and Obstetrics at Johns Hopkins Medicine.
The project—one in a series of multidisciplinary efforts meant to chip away at the mechanisms of aging and find therapies to help our bodies regenerate—is emblematic of Elisseeff’s penchant to ask bold questions and forge collaborations across a disparate array of fields.
A biomedical engineering professor at Johns Hopkins for 22 years, Elisseeff was recently named interim director of the Department of Chemical and Biomolecular Engineering. She is also the Morton Goldberg Professor of Ophthalmology.
Notably, she is the university’s only faculty member to be elected to all three national academies: the National Academy of Sciences (2023), the National Academy of Engineering (2018), and the National Academy of Medicine (2018).
After first using her biomaterials expertise to develop regenerative therapies and launch two successful startup companies, Elisseeff took a rare mid-career pivot into a complex field outside her specialty: immunology.
Today she is a leading expert on regenerative immunology—a burgeoning area of research that aims to harness the power of the immune system to heal the body—and her innovative collaborations with experts in cancer immunotherapy and computational biology, among other fields, have wide-ranging implications for tissue regeneration, cancer therapies, and diseases of aging.
“Jennifer is not afraid to come up with an idea that could very well be looked at as outlandish,” says Drew Pardoll, director of the Bloomberg- Kimmel Institute for Cancer Immunotherapy and oncology professor at Johns Hopkins Medicine. “Some of those ideas develop momentum and, all of a sudden, outlandish becomes transformative.”
The Immune System’s ‘First Responder’
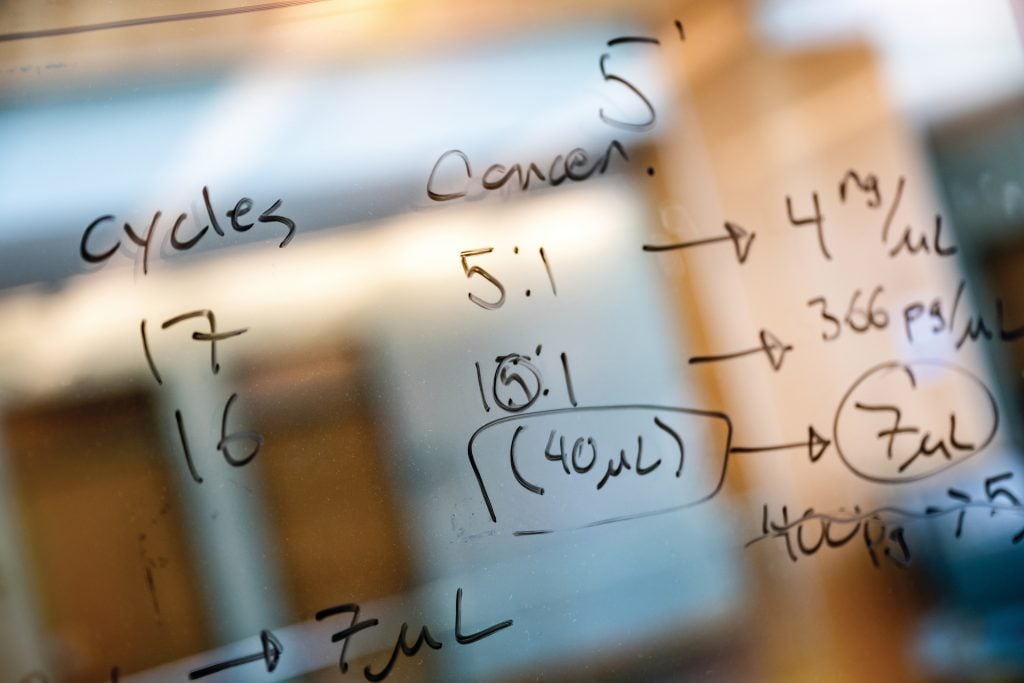
Elisseeff has been working on senescent cells for more than six years. In a seminal paper published in 2017 in Nature Medicine, she showed that eliminating senescent cells from an arthritic joint reduced pain and increased cartilage development. Her lab is now part of the NIH Common Fund Cellular Senescence Network, a collaborative program uniting cellular senescence researchers to study and publish public data on these important cells.
Her interest in senescent cells grew out of her fascination with the immune system. Senescent cells signal that the immune system has been activated, which occurs during tissue development and repair, as well as during harmful chronic inflammation.
She explains that while we most often think about the immune system in the context of vaccine efficiency or fighting infections, part of its job is to recycle cells that are no longer functioning as they should. The immune system also plays a role in the aging process. “The immune system is a first responder to tissue damage,” Elisseeff says, which has led her to ask: “How does aging change the immune environment and impact our ability to repair tissues?”
In partnership with bioinformatics colleagues at Johns Hopkins Medicine, Elisseeff has developed computational techniques to study how the immune system communicates—in young animals versus older animals—and how it changes and inhibits tissue repair. The goal, she says, is a new strategy for developing therapeutic targets for the illnesses of aging, such as neurodegenerative disease and frailty. This new strategy, she explains, will need to consider immune factors, such as diet, microbiome, history of infections, and comorbidities.
“[Typically] those factors aren’t part of the design process when you’re making new therapies for people,” she says. “How many therapies failed because those factors weren’t considered?”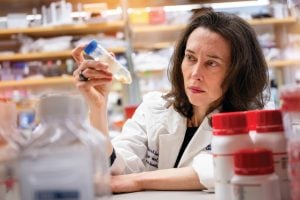
Elisseeff was the first engineer to collaborate with the Bloomberg-Kimmel Institute for Cancer Immunotherapy, and she has since recruited other biomedical engineers to join her efforts there. “Hopkins has amazing immunologists,” she says, “and not only basic science immunology, but also translational immunology, which is super exciting.”
Her current focus involves leading the institute’s program to engineer the tumor microenvironment, the complex ecosystem of cells, blood vessels, and other components that surround a tumor. She found that senescent cells play a role in these tumor microenvironments: When noncancer cells in a tumor were senescing, they could give the tumor a “senescence signature” that correlated with poor immunotherapy outcomes for cancer patients.
“She’s connecting dots that no other scientist has connected,” Pardoll says. “This is really very novel.”
Elisseeff’s senescence work has helped the researchers at the Bloomberg-Kimmel Institute to draw a clearer picture of the tumor microenvironment. “It had a major impact on our research into how a tumor microenvironment is organized, which, in turn, has broadened our thinking about how to therapeutically target these cells,” says Pardoll.
As Elisseeff learns more about senescent cells, and the other cells within tumors, she is aiming to engineer the ideal tumor microenvironment to make cancer immunotherapy treatments more effective—and make tumors more susceptible to those treatments.
“What environment promotes tumor growth and more resistance to therapies,” she says, “versus inhibiting tumor growth and increasing immunotherapy response?”
Improving Lives
When Elisseeff was a high schooler in the early 1990s, she could frequently be found in her father’s laboratory in the Department of Ocean and Mechanical Engineering at Florida Atlantic University in Boca Raton. A lover of nature with a penchant for science fairs, she was soon conducting her own basic research. In one particularly prescient example, the young Elisseeff studied how microbes impacted the chemical process on metal surfaces.
Even from a young age, she was intrigued by the collision of the natural and the synthetic. “Innovation happens at the crossroads,” she says.
On the recommendation of a favorite science teacher, Elisseeff attended Carnegie Mellon University, settling on an undergraduate degree in chemistry. While studying polymer chemistry, Elisseeff was introduced to the idea of combining polymers with biology—that is, biomaterials— bringing her closer to the medical field. Elisseeff pursued her PhD in biomedical engineering at the Harvard–MIT Division of Health Sciences and Technology, attended two years of medical school, and completed a postdoctoral program at the National Institutes of Health.
She joined Hopkins’ Department of Biomedical Engineering in 2001. “What is unique about biomedical engineering here is how it’s embedded in medicine,” she says. “I was attracted by the ability to bridge the different schools and start a new collaboration with physicians out of the blue, whether it be a cornea surgeon or a gynecologist studying fibroids or a cancer researcher.”
Her initial focus was engineering biomaterials, synthetic systems that could heal tissue wounds. She developed adhesive and biomaterial technologies to treat arthritis, restoring cartilage that had deteriorated in patients’ aching knees. The work led to her first startup, a company called Cartilix Inc. that was founded in 2004 and acquired by Biomet Inc. five years later. By then, Elisseeff’s interests had expanded into soft tissue regeneration, and she founded two more startups to translate her work.
A proponent of translating academic research into treatments for patients, Elisseeff recruited Jordan Green, the Herschel L. Seder Professor in Biomedical Engineering, to help establish the Translational Tissue Engineering Center (TTEC), a collaboration with the Wilmer Eye Institute, in 2010.
“Jennifer cares about the big picture,” says Green, who is now the department’s vice chair for research and translation and TTEC’s associate director. “It’s not just the science, but how the science can impact society.”
Following Elisseeff’s lead, Green became involved in the work of the ophthalmologists at Wilmer—a partnership he hadn’t expected. “She likes to bring different kinds of people together,” he says, noting that the TTEC floor is often filled with a mix of clinicians, medical students, residents, and researchers working together. “That environment can more easily lead to translational outcomes.”
Green has since founded two startups: Asclepix Therapeutics, which develops a peptide drug to treat wet age-related macular degeneration, and Cove Therapeutics, which develops nonviral gene therapy in the eye. “If it wasn’t for Jennifer’s leadership, I don’t think those would have happened,” he says. “It resonates with me that the research we do can lead to improvement to the quality of life for people who need help.”
It was the process of translating technologies to the clinical setting that made Elisseeff in 2013 begin to take an interest in the immune system —our body’s complex web of defenses—which she until then knew little about.
“We developed these therapies, but if you put them in an inflammatory environment, they’re not going to work,” she says. Without any formal immunology training, Elisseeff came to the conclusion that the immune system was key to successful regeneration. “That was a real clincher,” she says. “I had to learn some immunology.”
So, in an exceedingly rare move for an already-renowned researcher a dozen years into her career, Elisseeff embarked on a semesterlong sabbatical at the Swiss Federal Institute of Technology in Lausanne for an intensive immersion into the world of immunology.
Mentoring Women in Science
When she returned a few months later, Elisseeff connected with Kaitlyn Sadtler, a new graduate student with an interest in immunology who wanted to do a rotation in her lab. “Having had zero experience in bioengineering, I had no idea how big of a deal she was,” Sadtler says, laughing.
Soon, Sadtler had joined Elisseeff’s lab. Elisseeff, along with Pardoll, advised Sadtler on her PhD thesis. The resulting paper, a transformative work published in Science in 2016, showed that a specific type of T cell, previously known to combat parasitic microbial infections, was also central to wound healing.
Now a tenure-track investigator at the National Institutes of Health and chief of the Section on Immunoengineering, Sadtler says Elisseeff remains the only female principal investigator she has ever worked under. Elisseeff’s example as a role model—she once bought her mentee dinner when the graduate student looked wan after a long day in the lab—inspired Sadtler to mentor other women in science. “It’s hard to be what you can’t see,” she says.
Elisseeff considers her mentorship of women engineers one of her greatest accomplishments to date. “I’ve trained a lot of [women] students who are now faculty,” she says. “When you look at gender diversity in [engineering] departments, there’s usually not a great balance. My contribution of training women who now are in faculty positions around the world doing great work is important for the field.”
The Next ‘Crazy Challenge’
Elisseeff’s lab work isn’t her only race against time. She also competes in short-distance triathlons, races that include swimming, biking, and running segments, as part of her personal quest to age healthfully.
“It’s a sport where you have some diversity of different activities,” she says. “I enjoy mixing it up.”
When she’s not listening to music to stave off the tedium of the long, slow runs mandated by her triathlon training program (“It’s boring trying to be disciplined to go slower,” she says), Elisseeff sometimes finds herself musing on the engineering problems she’s trying to solve in the lab. Her next “crazy challenge” stems from her fibrosis work.
Elisseeff’s lab has data to suggest that T cells —adaptive immune cells known to combat outside invaders, such as germs and disease— might be recognizing fibrosis and perhaps, by extension, other types of tissue damage. If that’s true, it goes against basic immunology dogma because T cells aren’t supposed to be self-reactive: That’s considered an autoimmune disease. The notion is “a little bit controversial in some sense,” Elisseeff says.
“The adaptive immune system isn’t recognized as having a big role in tissue repair or a lack of repair,” she says. “This is a new way of looking at the role of the immune system in tissue repair that’s just very different.” But if Elisseeff can prove that T cells are recognizing fibrosis— which is no small feat—the finding could open up a huge new avenue of research into how T cells contribute to aging.
“I feel like I haven’t made my most important contribution yet,” she says.