Acclaimed as the “father of cardiopulminary resuscitation” (CPR), William B. Kouwenhoven devoted 50 years to inventing the procedures and devices to jolt a human heart back to life.
Even with the numerous testimonials, national awards, and articles about William Bennett Kouwenhoven, it is difficult to encounter the man behind the biographical facts. His resolute face, looking out at us from an old photo, with his ever-present pipe, tells us little of his personality, his motivation, even his spirit.
However, as one sifts through musty archives, glints of gold emerge. His colleagues and students called him “Wild Bill.” A native of Brooklyn, New York, where his Dutch ancestors had settled in 1623, he retained the classic Brooklynese patois in his speech, saying “loin” (learn) and “woik” (work). When receiving the prestigious Edison Medal from the American Institute of Electrical Engineers in 1962, he noted he had always felt an affinity for Thomas Edison, for both were of Dutch descent and interested in the effects of electricity upon human beings. The one difference, Kouwenhoven dryly added, was that he himself was concerned with “the applications of electricity in medicine,” while “Mr. Edison took an active part in the development of the electric chair.”
Still, it makes sense to review the main facts and considerable accomplishments of this remarkable man’s life. Or should we say “lives”—for there is more to Kouwenhoven than meets the eye.
THE SCHOLAR
As a college freshman in 1903 at the Polytechnic Institute of Brooklyn, Bill Kouwenhoven was curious about the relationship between electricity and medicine, and wrote English themes on the topic. Graduating with a BA in electrical engineering in 1906, followed by an MS in mechanical engineering in 1907, he taught at the institute until he married. He and Abigail then traveled to Germany, where he received a doctorate in engineering from the Karlsruhe Technische Hochschule in 1913. In 1914, he was appointed as an instructor in Electrical Engineering at the Johns Hopkins University.
It was a career move that changed Kouwenhoven’s life—and saved countless others. His advancement to professor and assistant dean in 1930 was notable in itself, as it was the University’s tradition at the time to have only one professor per department. He held that professorship for 24 years, while serving as Engineering dean from 1938 to 1954 and as chair of Electrical Engineering from 1942 to 1954.
Following his retirement in 1954, the professor emeritus started a new phase of his career— as a lecturer in surgery at the Hopkins School of Medicine, where he continued his pioneering research.
THE INNOVATOR
In the early years of the 20th century, electricity sparked the imagination of the American public. Everyone wanted to have offices and homes rewired for “the marvel of electrical lighting.” As a new college graduate, Kouwenhoven supplemented his teaching income by rewiring old houses in the summertime. “In those days, you didn’t have to have a license to do this work,” he recalled. “My partner and I made out pretty well.”

Behind electricity’s hoopla, danger lurked. By the 1920s, as electrical companies vied to string more wire and gain a greater market share, puzzling tragedies were occurring: Utility linemen who accidentally received even small jolts of electricity were suddenly dying from ventricular fibrillation (VF)—and no one knew why. The heart experiencing VF literally loses its rhythm and normal electrical activity, falling out of beat into a palsied state, unable to pump blood. The utility companies were determined to discover the connection.
In 1925, Consolidated Edison of New York (ConEd) selected the Hopkins School of Hygiene and Public Health as one of its exclusive research sites to study the effects of electricity on the human body. Much has been written on this stage of Kouwenhoven’s career (see timeline at right). However, beyond the sheer magnitude of his work, what stands out most is the single-minded perseverance of this man who devoted 50 years of his life to a single mission: saving lives through the application of electricity.
TIMELINE OF KOUWENHOVEN’S RESEARCH AND DISCOVERIES
1928
When the ConEd study begins at Hopkins, the principal investigator, neurologist Orthello Langworthy, surprises some by inviting to the team a professor of electrical engineering—Bill Kouwenhoven. In observing the effects of DC and AC shock on the heart, the team notes that low-voltage shocks cause ventricular fibrillation (VF).
1933
By applying a second surge of electricity (what Kouwenhoven calls a countershock) to a dog’s fibrillating heart, the team restores a normal heart rhythm. This landmark finding, called defibrillation, opens the door to a radically new approach to cardiac care.
1933-1947
The team applies its defibrillation discovery to open-chest cardiac resuscitation techniques. The research results in the first successful use of an electric defibrillator on a human heart, by Claude Beck ’21 MD, in Cleveland in 1947. Kouwenhoven is still dissatisfied. “Linemen were still dying from electric shocks, and what could be done to save them?” he writes. “Even if a surgeon could be assigned to every line truck, the opening of the chest is still a major operation that should be performed only in a hospital.”
1951
Through the cooperation of the medical school’s Department of Surgery, and an Edison Electric Institute grant, Kouwenhoven begins research into the development of a closed-chest defibrillator. In his own words, it “would be portable, effective, simple to operate, and the shock of which could be sent through the chest of an individual whose heart was beating normally, without fear of injury.”
1954
G. Guy Knickerbocker ’54, ’71 PhD, who has just received his undergraduate degree in electrical engineering, joins Kouwenhoven’s team.
1957
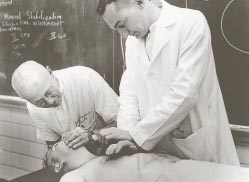
The team unveils its prototype— the Hopkins A-C Closed Chest Defibrillator. Weighing in at a bulky 200 pounds and mounted on a rolling cart, the machine delivers a defibrillating countershock of 5 amperes at 440 volts for .25 second via two main electrodes. After extensive animal testing by the team, on March 17 at the Hopkins Hospital, admitting resident Gottlieb C. Friesinger II, MD (now a Hopkins trustee emeritus) became the first to use the machine on a patient, a 42-year-old man. According to Kouwenhoven, “ About 3:30 a.m.…his heart went into defibrillation. When the countershock was sent through his chest 72 seconds later, his heart was defibrillated and he lived again.”
1958
James R. Jude, MD, a protégé of famed Hopkins cardiovascular surgeon Alfred Blalock, MD, joins the team. Knickerbocker notices that placing defibrillator paddles on a dog’s chest causes a rise in blood pressure. Kouwenhoven, Knickerbocker, and Jude experiment with different hand positioning and rhythms, and discover that through a combination of “closed chest cardiac massage” and “artificial respiration” that they could restore 40 percent of the normal blood circulation and in effect, resuscitate patients in cardiac arrest. They call this process cardiopulmonary resuscitation (CPR).
1959-1960
Twenty Hopkins patients in cardiac arrest are administered CPR, and are all resuscitated. Kouwenhoven, age 74, writes, “This was the breakthrough we were looking for.”
1961
Kouwenhoven’s team, with the support of the Mine Safety Appliance Company of Pittsburgh, introduces the first truly portable defibrillator, which weighs 45 pounds and fits into a small plastic suitcase. Kouwenhoven, Jude, and Knickerbocker publish their findings on external cardiac compression in a landmark article in the Journal of the American Medical Association
THE GENIUS AFFIRMED
In 1969, in recognition of his contributions to medical science, Kouwenhoven was awarded the first honorary degree ever conferred by the School of Medicine. He received many other honors, including the Hektoen Gold Medal from the American Medical Association. In 1973, two years before his death, he was awarded America’s most prestigious biomedical prize, the Albert Lasker Award for Clinical Medical Research. The award citation read, “We salute you, Dr. Kouwenhoven, for your ageless genius…” When Kouwenhoven died at the age of 89, the New York Times obituary observed that he had “developed the basic cardiac treatment devices and procedures used worldwide.”
THE “WILD BILL” OTHERS KNEW
There’s yet another way to meet the real Kouwenhoven—through interviews with colleagues, family, and acquaintances.
“That was an exciting time.”
James R. Jude, MD came to Hopkins in July 1953 to train as a surgeon. In 1961, he became an instructor in the School of Medicine, and later served as an assistant professor in Surgery. He left in 1964 to teach at the University of Miami School of Medicine, where he also served as head of Thoracic and Cardiovascular Surgery. In 1971, he opened a private practice in Miami, from which he retired in 2000.
“When I was an intern at Hopkins, I carried out research I had started in medical school on hypothermia, its effects on the heart, and its use in surgery. From the upper level of the building, I kept noticing the sounds of high-voltage electricity, like lightning and thunder. That’s where I first met Dr. Kouwenhoven.
“In 1955, I spent a year in the new Blalock Building laboratory, and he worked at the other end of the floor. As part of my research with hypothermia, I was looking at defibrillation techniques. Guy Knickerbocker, then a doctoral student in Electrical Engineering under Dr. Kouwenhoven, came over to help me out. Through him, I got to know Dr. Kouwenhoven and his lab.
“While working at NIH for two years, I kept in touch. In 1957, I got a call from Guy Knickerbocker saying that he had found that firmly placing the defibrillator paddles on a dog’s chest had caused a rise in blood pressure. When I returned to Hopkins in 1958, I was an assistant resident in cardiac surgery and had an opportunity, under controlled circumstances, to apply this technique of external cardiac compression to patients. After developing a number of clinical cases under safe means, we began teaching this technique to local firefighters, in tandem with mouth-to-mouth resuscitation.
“The development of CPR was a group effort. You have to understand that before this and defibrillation, the only way to save a patient going into cardiac arrest was for a thoracic surgeon to open the chest and physically squeeze the heart—sometimes repeatedly, so that we used to joke that some patients needed a zipper!
“I continued working with him on a part-time basis until I left Hopkins. That was an exciting time—cardiac surgery was just beginning. They may have seemed like small steps, but they were important steps.”
“I merely gave him the tool.”
Gil Kaisler, a Baltimore native, earned his BS in mechanical engineering at Hopkins in 1944. Following a stint in the Navy, he returned to Baltimore and worked for Western Electric. He attended Hopkins at night to earn a second BS, in electrical engineering, in 1952, and studied with Kouwenhoven. Kaisler was then hired by the Consolidated Gas and Electric Light and Power Company of Baltimore (now BGE) as an investigator in its research department. He retired in 1988.
“While working in the research department, I studied electrical shocks and hazards. I was following up on the death of one of our workmen who died of fibrillation after being shocked by a 120-volt electrical circuit. In 1953, the company’s board of directors provided a $10,000 grant to investigate how to counteract the effects of defibrillation.
“One day, my boss called me into his office and asked me, ‘What is the smallest portable AC generator you can come up with?’ When I asked why, he said, ‘We want to stop a heart.’ From my Navy experience working on radios, I’d been kicked by electric discharges many times. So I said, ‘build a capacitor discharge device.’
“During my research with fibrillation, I had gotten hold of a study with data on time duration, voltage, and the probability of death from various electric currents. It said that there was a 99 percent probability of death from a one-half cycle electric current of 50 milliamps. So the size of the device we wanted was the then-current equivalent of a capacitor discharge analogous to a 60-cycle wave. Since the electric skin resistance of the body was 10,000 ohms, we’d need about 500 volts with the duration of whatever the capacitor discharge was from the device.
“I recommended that we use ten 45-volt radio batteries and eight electrolytic capacitors, put through an antenna switch that had the capacity to withstand 500 volts between segments—which amounted to about 200 joules. The next I knew, they were building this thing in our research department’s laboratory. They used heavy half-inch plywood for the box, but it was portable, about 18 inches square.
“We were told to put this box into my 1950 Plymouth and take it to Hopkins. We met Dr. John Franklin, the co-sponsor of the BG&E grant, who was then working with Dr. Kouwenhoven. Dr. Franklin had an anesthetized dog on its back and gave it a shock, fibrillating the heart. Then he used my device, and on the third try, it stopped the fibrillation, and the heart resumed beating normally, as we could see on the oscilloscope.
“Dr. Kouwenhoven had the great idea to stop the fibrillating heart and then restart it. I merely gave him the tool to do it, by developing the circuitry. You know, it’s funny, but I don’t know if they ever tried any other combination of capacitor or voltage. It was always 200 joules. Many years later, I was working on a defibrillator made by a British electronics firm, and sure enough, it had the same voltage, same capacity, same 200 joules! It was my design. So I’m proud of my contribution.”
“I was entranced by what I saw.”
G. Guy Knickerbocker received a full scholarship to attend Hopkins, where he studied electrical engineering under Kouwenhoven, graduating with a BS in 1954. After serving as a researcher with him for 17 years, Knickerbocker earned his doctorate in electrical engineering in 1971. The next year, he moved to Philadelphia and worked for the nonprofit Emergency Care Research Institute. He retired in 2000.

“There was no question that Dr. Kouwenhoven was a fascinating guy. To a certain extent, the approbation of ‘Wild Bill’ carries some credibility. Being brought up in Brooklyn, he was colorful. On the other hand, he had a generous side.
“I took his last lecture course in electrical power in my senior year. John Gitt, a friend and classmate, was a lab assistant when Kouwenhoven was conducting his electric shock studies at the Hospital. Over coffee at Levering Hall, John would tell me about the things that were going on with Dr. Kouwenhoven’s electrical experiments with defibrillation. I was really intrigued by this, so he arranged for me to accompany them on one of their experiments. I was entranced by what I saw.
“I wanted to do my graduate studies at Hopkins. Dr. Kouwenhoven needed an assistant for a research project on plastics that he was directing at Homewood, and offered me the position that allowed me to pursue my master’s in electrical engineering. He would go down to the Hospital and do experiments one or two afternoons a week, and I would go, too, and help him out.
“I was a perennial graduate student, so in the meantime I was working up to full-time at the Hospital on the defibrillation problem. At the same time, we were trying to characterize the adverse and beneficial effects of electricity on the heart. There was a mix of studies all wrapped in there together, funded by different private entities.
“We worked on the original unit that rolled around on a cart— it was basically a big transformer that took voltage from an outlet and jacked it up to about 440 volts, applying a shock for about a quarter of a second. After our publication of research on cardiac resuscitation, we went on to develop a smaller portable device that could be used for field emergencies.
“For the defibrillator to fire, you had to apply the paddles to the chest of the test animal rather forcefully. We were always measuring arterial blood pressure so that we could see that there were effective contractions. We noticed that when we applied pressure to the animal’s chest, there appeared to be an elevation of the pressure within the arteries. We wondered whether that was doing any good.
“During a later experiment on a fibrillating test animal that we did not expect to recover, we applied pressure to the chest and then, five minutes later, applied the defibrillator and revived the animal. It was extraordinary to have this kind of recovery. This event was pivotal in giving us a sense that enough blood had to be flowing to slow down the dying process. Through the evidence we pieced together, we saw that something good was happening. Jim Jude’s participation was also instrumental at this point in applying this technique to cardiac patients.
“I don’t know at the time that I had any strong feelings that our research was going to be earthshaking. I had friends who had said, after we published our findings, that we’d be going to Norway for the Nobel Prize. But I could never think in terms of that context at all. I don’t consider myself an inventor of CPR. Everybody stands on the shoulders of other people.”
“A reverence for utility”
Nick Kouwenhoven is a son of Kouwenhoven’s only child, the late William G. Kouwenhoven ’44, ’49 MSE. Nick works for Tessco Technologies in Baltimore, where he manages a family of products for the wireless and cellular telephone industry. Nick’s older brother, William B. Kouwenhoven ’85 A&S, ’86 MA, lives in California.

“My grandfather was an extremely intense and competitive man. When I was a little boy, we used to play dominoes. He had no qualms about destroying me in a game; for him, it was simply a matter of that’s how you played—to win. And that’s how you learned. As a teacher, he was known for being demanding, but I also have learned that he secretly paid for kids who showed promise to go to school. But he never made anything of that. He was also an excellent storyteller who would use humor to illustrate a point.
To me, he was somewhat like a modern Prometheus—he turned on the juice and people came back to life. “He was tough, tenacious—demanding excellence at every point. He spent 40 years of his adult life trying to solve a single problem: the development of the defibrillator and CPR. He didn’t stop until his failing eyesight prevented him from going to work. He was really a pioneer of today’s life sciences professional.
“He sailed throughout his life, beginning on waters around Long Island as a boy. For many years he kept a 43-foot Alden schooner, The Wilabil, at Gibson Island. The family lived on the boat every summer, and often took his colleagues and graduate students out for a sail on the Chesapeake Bay. He took care of the boat himself, not an easy thing to do, especially when you’re 80 years old. He even had his wife crank him up the mast to fix the rigging!

“If my grandfather built something, say a dinghy, and he wasn’t satisfied with the available tools, he built the tools himself. He was a tinkerer, a builder of things from the ground up. When he was first invited to take part in the electrical studies at Hopkins in the 1920s, they apparently chose him because they thought he had a creative mind and could figure out a different way to solve the problem.
“He was a complicated man; he could be charming and then reveal his underlying stubborn nature. He had a strong faith and was a student of the Bible, though he was not a church-goer. He got along very well with the leading doctors at Hopkins, who ultimately gave him access to medical labs—and an honorary MD. As it turns out, so many thousands of people’s lives have been saved over the years by the work of this Hopkins team that it might have been suitable to consider the team’s work for a Nobel Prize.
“My grandfather was always trying to improve upon his work. Many family dinners included his graduate students, and the conversation frequently turned to the subject of their work. He had a reverence for utility—you put in an honest day’s work, you use your brain, and you just keep moving forward. He excelled as a teacher and administrator, but in the far grander scale, he did something to help countless people. That was his gift.”
An Appealing Continuity
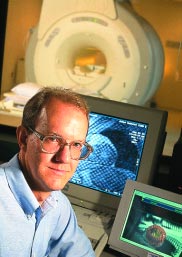
In 1981, the Whiting School established the William B. Kouwenhoven Professorship in Electrical Engineering, an endowed chair to honor the memory of this extraordinary individual. The Kouwenhoven Professorship is held by Jerry L. Prince, who joined Hopkins in 1989. He is also associate director for research at the Center for Computer Integrated Surgical Systems and Technology and holds joint appointments in Mathematical Sciences at the Whiting School and in both Radiology and Biomedical Engineering at the School of Medicine. In 1993, he was named a Presidential Faculty Fellow by the National Science Foundation, and in 1997, he was honored as Maryland’s Outstanding Young Engineer.
Prince co-developed HARP MRI (harmonic phase magnetic resonance imaging), which enables doctors to see the condition of heart muscles in seconds, with potential uses in screening and monitoring cardiovascular disease. His current research interests include image processing and computer vision with primary application to medical imaging.
Serving as the Kouwenhoven Professor is “very meaningful for me,” says Prince, “and not only for the prestige. First, the previous holder of the chair was Charles Roger Westgate, who recruited me to come to Hopkins, and was a mentor of mine. Second, the work that Kouwenhoven did on the heart is very important to me, because my biggest research area is imaging the heart using magnetic resonance. So there’s a continuity that I find appealing— I hold a chair honoring a person who did fundamental and important research on the heart. His first use of the closed-chest defibrillator in surgery occurred in 1957, the year I was born. I hope to do as important work some day.”




