Digital twins—virtual replicas that simulate a patient’s unique cardiac structure and function—hold promise for predicting heart problems, but they aren’t yet reliable enough for clinical use. Two Johns Hopkins civil and systems engineers are applying their expertise in computational modeling to change that, working to make digital twins of human hearts accurate enough to reliably predict which patients will suffer dangerous heart rhythm disruptions that can lead to sudden cardiac death.
Supported by the National Science Foundation, Dimitris Giovanis, an assistant research professor, and Somdatta Goswami, an assistant professor, are co-PIs on a team that is developing new ways to correct errors in existing heart digital twins. Led by principal investigator Mauro Maggioni and co-principal investigators Natalia Trayanova and Yannis Kevrekidis, they aim to transform the twins from promising research models to clinical tools that could improve procedures like cardiac ablation, where surgeons precisely destroy small areas of heart tissue to treat dangerous arrhythmias, and ultimately save lives.
“Sudden cardiac death is the leading cause of natural deaths worldwide, and it can sometimes happen within just an hour of symptom onset. A major challenge in effective prevention is figuring out which patients are at risk. If we can improve how we predict and treat heart conditions using digital models, we could save lives and improve care for people living with serious heart problems,” said Giovanis.
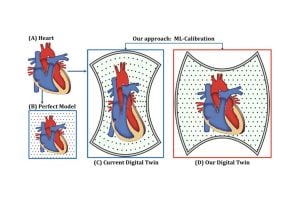
The team’s approach starts with a 3D digital heart model created using patient scans and standard modeling. Their key innovation comes next: using advanced mathematics, digital simulations, machine learning, and patient data to fine-tune the models. Machine learning compensates for data limitations and biological uncertainties, while advanced mathematical modeling corrects errors in the replica. They say that the resulting digital twin will be better at predicting what’s happening inside a patient’s heart.
“Enhancing cardiac digital twins will make ablation procedures—removal of tissue—for people with heart arrhythmias more accurate and efficient. Reliable, patient-specific replicas will allow doctors to plan precisely where and how to intervene, potentially shaving hours off of procedures and improving outcomes for those with heart conditions,” says Goswami.
Improved digital twins could transform not only cardiac ablation but medical care more broadly.
“Imagine doctors running any number of virtual experiments, testing new drugs, or planning surgeries on the twins—without ever putting the actual patient at risk,” said Giovanis.
He envisions this technology as a tool to answer questions about the progression of an individual’s medical diagnosis, determine who’s most likely to benefit from a therapy, and avoid unnecessary treatment.
As the next step in the research, the team plans to test and refine their models using a larger group of patient samples.
“We want to make digital twins ready for use in real clinics during everyday practice to support doctors in making better, faster, and more informed treatment decisions for patients,” Giovanis said.