Ankur A. Butala, M.D.
Assistant Professor of Neurology, Movement Disorders, Neuropsychiatry
Dr. Ankur Butala specializes in the care of persons with complex neuropsychiatric conditions including persons with advanced Parkinson Disease or other movement or neurodegenerative disorders. Upon graduating a selective Physician-Scientist program at Albany Medical College, he joined the University of Massachusetts in an uncommon residency in both Neurology and Psychiatry. Dual-trained neuropsychiatrists such as Dr. Butala have experience with: Parkinson Disease and atypical Parkinsonism, Huntington Disease, Ataxia, Dystonia, early-onset dementia, traumatic brain injury and chronic traumatic encephalopathy, autism spectrum disorders, medication refractory mood and psychotic disorders, epilepsy and functional neurological disorders.
In residency he developed an interest in circuit-models of brain function and how non-pharmacological approaches such as Neuromodulation and brain stimulation may be used to address treatment resistant conditions. Consequently, he joined Johns Hopkins University School of Medicine as a Clinical and Research Fellow from 2015 to 2018, where he developed a skill set including deep brain stimulation, non-invasive brain stimulation (tDCS) and measurement of eye movements.
Currently Dr. Butala's clinical and research interests are in the diagnosis and management of persons with advanced Parkinson Disease, movement disorders and neuropsychiatric conditions using neuromodulation, cannabinoids and entheogens.
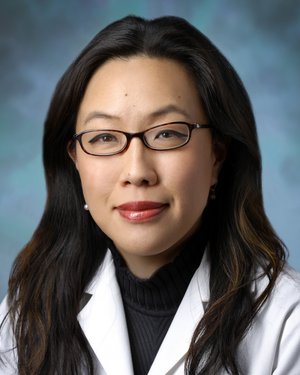
Esther S. Oh, M.D., Ph.D.
Associate Professor of Medicine, Co-Director, Johns Hopkins Memory and Alzheimer's Treatment Center
Dr. Esther Oh is an associate professor in the Division of Geriatric Medicine and Gerontology, and an associate director of the Johns Hopkins Memory and Alzheimer’s Treatment. Dr. Oh is interested in developing biological markers for pre-clinical stages of Alzheimer's disease (AD). Her current research involves using transgenic models of AD to develop peripheral injections of monoclonal antibodies against amyloid-beta as a tool to detect a level of amyloid-beta that would be correlative to the amyloid-beta level in the brain.
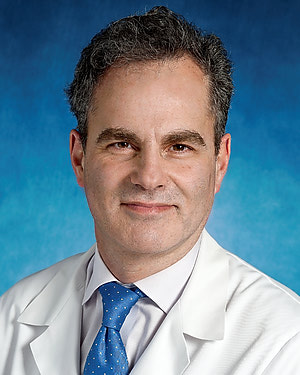
Robert D. Stevens, M.D.
Associate Professor of Anesthesiology and Critical Care Medicine; Director, Division of Informatics, Integration, and Innovation
Dr. Stevens is fellowship-trained and board-certified in critical care medicine, neurocritical care, and anesthesiology. He treats patients with critical illnesses such as sepsis, ARDS, acute kidney injury, traumatic brain injury, and stroke. He has special expertise in the resuscitation of patients after cardiac arrest. Following medical studies, Dr. Stevens received postdoctoral research training in molecular neurobiology, cellular electrophysiology, advanced magnetic resonance imaging, and brain mapping. He holds faculty appointments in the Johns Hopkins Institute for Cell Engineering, Institute for Computational Medicine and the FM Kirby Center for Functional Neuroimaging. Dr. Stevens is on the Council of the European Society of Intensive Care Medicine and chairs the Committee on Computational Critical Care Medicine at the SCCM. He is an Associate Editor of the journal Thorax, and serves on the Editorial Boards of Critical Care Medicine, Neurocritical Care, and Frontiers in Neurology.
Dr Stevens’ vision is to deploy Precision Medicine for the benefit of critically ill patients. His research aims to discover and validate patient-specific biological signatures associated with trauma, surgery and acute conditions such as stroke, cardiac arrest, and sepsis. To achieve this, he engages with an interdisciplinary group of basic and systems neuroscientists, biomedical and computer engineers, biostatisticians, data scientists, and neuroradiologists. Dr Stevens is the principal investigator of the Neuroimaging for Coma Emergence and Recovery (NICER) project, which examines MRI features of the brain connectome to enhance classification and prediction in patients recovering from severe brain injury. Other projects from Dr Stevens’ group analyze features captured through neurophysiologic monitoring, structural and functional MRI of the brain, serum biomarkers and wearable sensors, with the goal of enhancing classification and prediction in vulnerable, acutel ill patients. In the lab, Dr Stevens’ group studies molecular and cellular determinants of injury and recovery in experimental models of traumatic brain injury, stroke, and sepsis, with a special emphasis on neuro-immunological responses and cellular regeneration.
Peter M. Abadir, M.D.
Associate Professor of Medicine, Geriatric Medicine
Peter Abadir research focuses on the renin-angiotensin system (RAS), a signaling pathway that regulates blood pressure and has been linked independently to both aging and inflammation. His team is particularly interested in changes in RAS that occur with aging. They also study signal transduction and the role of the crosstalk between angiotensin II receptor in aging and are interested in understanding the function of angiotensin II in the process of vascular aging.