
A master’s student in Applied Mathematics and Statistics at the Whiting School of Engineering is part of a team developing Miraheart, an innovative non-invasive device to monitor infants’ heart activity using light sensors. Adrian Severino is refining the device’s light emission system to improve its ability to detect early signs of congestive heart failure.
The Miraheart project, which originated in the Department of Biomedical Engineering’s Center for Bioengineering Innovation and Design (CBID) program, uses non-invasive photoplethysmography (PPG) technology to track heart activity and assess central venous pressure (CVP) in infants and children with heart defects. This enables parents to monitor their baby’s health at home shortly after birth. The team won the Southwest National Pediatric Device Consortium’s $25,000 Pediatric Device Prize at the Rice Business Plan Competition last May and took third place at the Heartland Challenge Startup Competition, held last April at the University of Arkansas.
Severino joined the team to use mathematical modeling to de-risk and assess the technology’s feasibility before significant time and money were invested in developing a prototype, according to Danielle Gottlieb Sen, project lead and a pediatric cardiothoracic surgeon at Johns Hopkins University.
“Having Adrian on board as our math expert has been incredibly valuable—his work was essential in identifying the shortcomings of the technology we initially selected for our clinical needs, ultimately leading us to change direction,” Sen said.
Severino is modeling how light travels through tissue, focusing on how it moves through a 3D model of an infant’s neck and interacts with the internal jugular vein (IJV)—a major blood vessel that carries deoxygenated blood from the brain, face, and neck back to the heart—a region not extensively studied in this context.
“We aim to understand how efficiently our device detects and measures light that reaches the interior jugular vein,” he said, emphasizing the vein’s critical role in assessing a baby’s heart condition.
The device’s innovative design uses LED emitters and precise detectors to measure how much 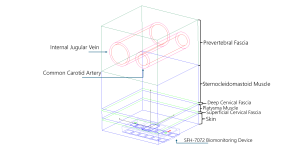 light passes through the baby’s tissue and returns. It translates this data into a special wave pattern called a photoplethysmography or PPG waveform, that provides crucial information about blood pressure in the central veins. This reading helps parents and physicians monitor how well the heart is pumping blood.
light passes through the baby’s tissue and returns. It translates this data into a special wave pattern called a photoplethysmography or PPG waveform, that provides crucial information about blood pressure in the central veins. This reading helps parents and physicians monitor how well the heart is pumping blood.
To optimize how the device captures this important information, Severino is using Monte Carlo simulations, a statistical method that models random processes to understand complex systems.
“By simulating light particles, as they travel through various tissue layers, we can estimate how much light reaches the target area and returns to the detector, offering a powerful tool for predicting photon behavior as it interacts with biological structures,” he said.
Another crucial aspect of the team’s work involves determining the optimal placement of the device’s sensors on the baby’s body.
“If the sensor and the light emitter are positioned too closely together, we risk detecting stray light that hasn’t interacted with the target vein, which is crucial,” Severino said.
In the initial round of testing, the team discovered that the sensor detected only 1.5% of the emitted light passing through the tissue. This weak signal highlighted the need to enhance the tissue’s light transmission and increase the intensity of the light source for more accurate results.
By adjusting the placement of the light source directly beneath the target area, they improved the focus of the light, increasing its interaction with the internal jugular vein while reducing scattering. Severino said that this adjustment significantly enhanced the device’s accuracy and reliability in monitoring central venous pressure.
“Each simulation run and challenge I encountered deepened my understanding of applied mathematics and brought me closer to the goal of leveraging technology to make a difference in infant health care,” he said.
The project is supervised by Dan Naiman, professor and associate head of the Department of Applied Mathematics and Statistics, Youseph Yazdi, assistant professor of biomedical engineering and executive director of the Center for Bioengineering Innovation and Design, and Danielle Gottlieb Sen, Pediatric Cardiothoracic Surgeon at Johns Hopkins University.